In-hospital cardiac arrest (IHCA) survival rates are astonishingly inconsistent between different healthcare institutions. According to data collected prior to COVID-19, IHCA survival varies from 9.2% to 37.5% — even after adjusting for age and other comorbidities.1 This suggests that more consistent adherence to proven best practices could prevent thousands of deaths per year.
One such practice is the designation of a resuscitation champion — a dedicated staff member with a clinical background who is passionate about improving resuscitation practices at every level of the hospital. In fact, according to a nationwide survey of data from 130 hospitals, those with a recognized resuscitation champion had nearly three-fold greater odds of being in a higher IHCA survival category.1
So, let’s say you have someone in mind who might be a good fit at your hospital. What exactly does this Code Blue guru do? Keep reading to learn the three key responsibilities of a resuscitation champion.
1. Identify Gaps in Code Blue Care
Perhaps the most important responsibility for a resuscitation champion is to gain a holistic understanding of Code Blue care practices across the hospital in order to spot areas in need of improvement. To accomplish this goal, resuscitation champions may assist in ongoing data collection process by:
- Directly gathering information from IHCA events per The Joint Commission’s revised requirements for resuscitation.
- Collecting feedback from clinical staff involved in events — especially those that went suboptimally. What lessons can be learned? Were there unforeseeable circumstances that contributed to poor outcomes or could process changes have improved the result?2
- Organizing and presenting data to the resuscitation committee.
But regardless of data collection methods, the following responsibilities are essential for a resuscitation champion to identify gaps in Code Blue care:
- Keeping up with evolving resuscitation best practices from the American Heart Association (AHA), The Joint Commission (TJC), the National Academy of Medicine (NAM), the International Liaison Committee on Resuscitation (ILCOR), and other trusted organizations.
- Reviewing actual cases and data from across the hospital on a regular basis — at least quarterly but preferably monthly — and comparing against best practices.1
- Using collected data to identify positive and negative trends and flagging areas that are in need of improvement — from clinical point of care to system-wide considerations and everywhere in between.
2. Spearhead Quality Improvement Initiatives
Once a resuscitation champion understands which practices, processes, or tools are in need of improvement, they must next lead the charge in effecting positive change in those areas. Key elements of this responsibility include:
Recommending practical quality improvements (QI)
- What specific improvements can be made — and how?
- What good habits can be standardized?
- What is the most effective way to communicate changes to clinicians, administrators, and other key stakeholders?
This can and should be a collaborative process, undertaken as part of a multidisciplinary committee intimately familiar with current IHCA practices.
Supporting QI at every level
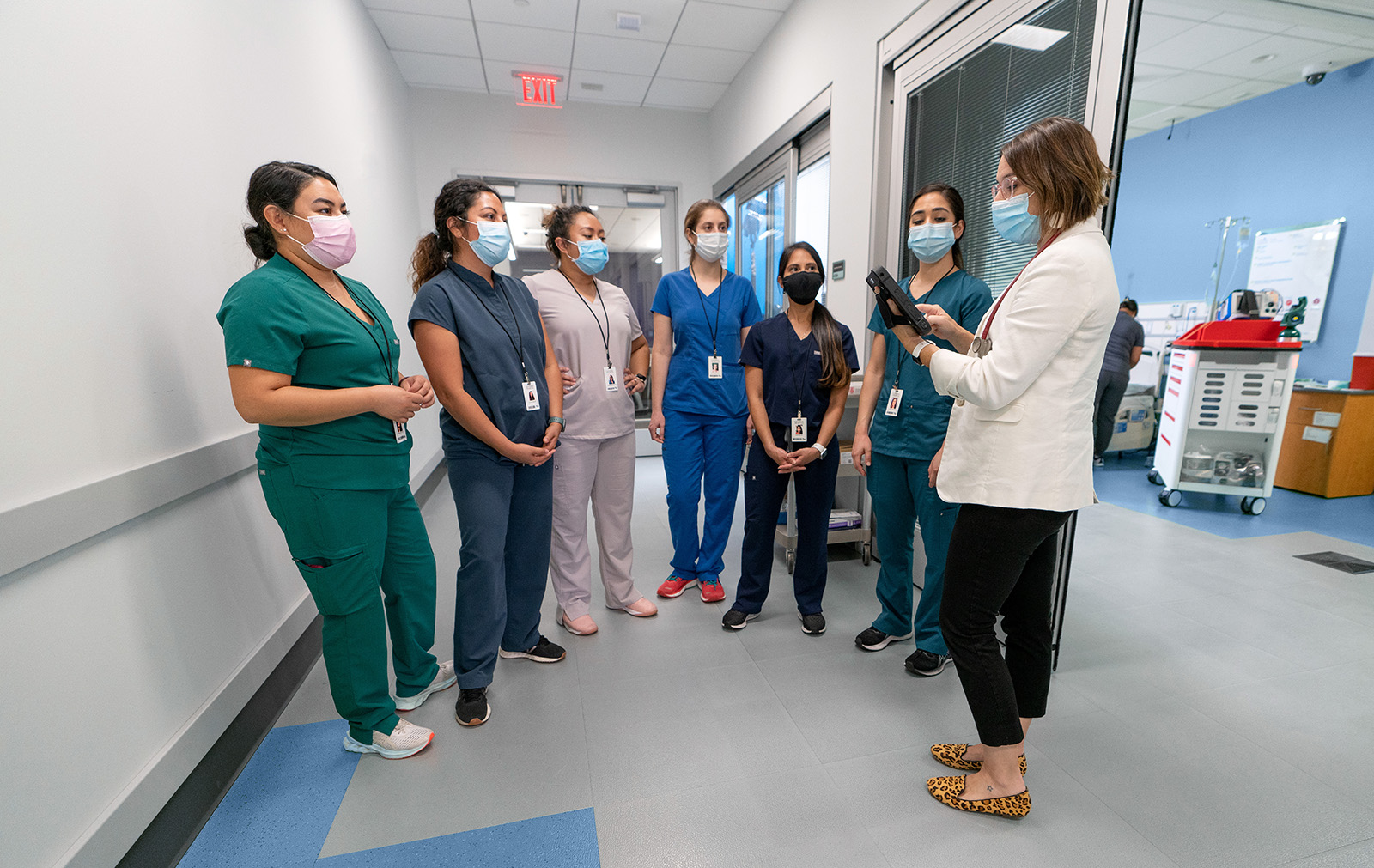
The resuscitation champion plays a vital role in driving lasting clinical practice improvements. Clinical staff are more likely to buy into QI efforts when there’s an invested and energetic champion with a strong clinical background at the helm.
The resuscitation champion should also actively promote all conclusions and recommendations reached by the resuscitation committee (including institutional or systemic changes) and clinical training that adheres to The Joint Commission’s revised resuscitation requirements.3
Tracking the results of QI initiatives2,4
- Are the changes bringing about positive results, such as improved survival rates, neurological outcomes, response speed, adherence to best practices, quality of cardiopulmonary resuscitation (CPR), or other factors known to impact outcomes?
- Were there unexpected negative outcomes or no change at all?
Documenting progress is essential to ensure Code Blue care improvement initiatives are always being directed (or redirected) in the right direction.
3. Be the Go-To Code Blue Advocate and Expert
One of the most important roles a resuscitation champion plays is subject matter expert. Every hospital needs a point person who clinical staff can ask resuscitation-related questions, such as:
- What are our hospital-specific resuscitation policies and protocols?
- What are the latest changes and QI initiatives being implemented?
- What are the latest guidelines and requirements from AHA, TJC, NAM, ILCOR, and other organizations?
The resuscitation champion also acts as an advocate by:
- Promoting IHCA as part of the hospital’s quality monitoring portfolio.
- Lobbying for additional acute and post-resuscitation care resources as needed.
- Being an active and engaged leader in all resuscitation committee activities and sessions.
We’re Here to Help
CoDirector® Software from Nuvara® can help Code Blue response teams more easily implement IHCA best practices and QI changes by:
- Empowering responders to digitally document all interventions in real time.
- Allowing your hospital’s resuscitation algorithms and medication dosing protocols to be customized and easily updated.
- Providing an interactive dashboard of automated timers that enables clinicians to pace recurring actions and monitor CPR quality in the moment.
- Delivering out-of-the-box, automatic event reporting for key clinical quality indicators and exportable data for deeper data analysis.
- Automatically creating both “hot” and “cold” debrief reports.

Related Articles
See CoDirector in action
Learn how CoDirector Software can help your hospital improve factors that impact resuscitation outcomes.
References
-
Chan, P. S., Krein, S. L., Tang, F., Harrod, M., Kennedy, M., Lehrich, J., & Nallamotu, B. K. (2016). Abstract 242: Resuscitation practices associated with survival after in-hospital cardiac arrest: A nationwide survey. Circulation: Cardiovascular Quality and Outcomes, 9(suppl_2). https://doi.org/10.1161/circoutcomes.9.suppl_2.242
-
Becker, L. B., Aufderheide, T. P., & Graham, R. (2015). Strategies to improve survival from cardiac arrest. JAMA, 314(3), 223. https://doi.org/10.1001/jama.2015.8454
-
Edelson, D. P., Yuen, T. C., Mancini, M. E., Davis, D. P., Hunt, E. A., Miller, J. A., & Abella, B. S. (2014). Hospital cardiac arrest resuscitation practice in the united states: A nationally representative survey. Journal of Hospital Medicine, 9(6), 353–357. https://doi.org/10.1002/jhm.2174
-
McCoy, M. A., & Schultz, A. M. (Eds.). (2017). Exploring strategies to improve cardiac arrest survival. National Academies Press. https://doi.org/10.17226/23695