When in-hospital cardiac arrest (IHCA) occurs, a resuscitation response team is often all that stands between the patient and serious harm or death. These courageous clinicians are the backbone of any hospital — those whose skills shine under the immense pressure of a dire, emergent situation.
But these real-life heroes don’t just magically appear as a fully-formed group knowing how to collaboratively execute advanced resuscitation techniques. The most effective code teams are built thoughtfully and systematically. They’re trained with purpose and intent using techniques supported by scientific data.
Although every institution is different, there are a few common considerations you’ll want to keep in mind when creating a Code Blue team. Keep reading to learn how to assemble and empower the best resuscitation response team for your hospital.
Assembling your resuscitation response team
First, you’ll need to figure out which staff members will become trusted, pager-wielding responders on your code team. Start by listing out essential roles, including required credentials (who do you need?). Then, supplement that with your “wish list” of additional members who could add value to the team (who do you want?). And finally compare those lists against the available staff at your institution (who do you have?). Here’s what the process might look like for a typical hospital.
WHO DO YOU NEED?
- Medical Doctor (MD)
- Registered Nurse (RN)
- Enough hands to support Advanced Cardiac Life Support (ACLS) measures
- Staff members with active American Heart Association (AHA) ACLS and Basic Life Support (BLS) certifications
WHO DO YOU WANT?
Some variability comes into play when you start thinking about the specific types of MDs, RNs, or other roles that would ideally attend regularly, such as:
- Emergency Department (ED) or Intensive Care Unit (ICU) MD
- Critical Care or ED RN
- Pharmacy representation
- Respiratory Therapist (RT)
- Surgery representation
- Anesthesia representation
Depending on several factors, this list will change:
- Smaller institutions might have trouble supporting consistent attendance for an ED- or ICU-specific MD or an ED- or Critical Care-specific RN.
- In larger hospitals, Surgery and Anesthesia representatives are often considered core responders because there are simply more of them to go around. Surgery typically places chest tubes and central venous catheters and performs cricothyrotomies, while Anesthesia usually helps with more advanced airways.
- At teaching hospitals, however, Anesthesia usually performs all intubations.
- Your location also plays a role, as credentials and scope of practice for all healthcare providers changes from state to state. For example, RTs are able to perform intubations and draw arterial blood gases in some states but not others.
WHO DO YOU HAVE?
Perform a full assessment of the current staff at your institution:
- Who has the necessary certifications?
- Which roles on your “need” and “want” lists are already represented?
- How many of each role are available at various shifts to ensure 24/7 coverage?
- How are these staff members distributed across the physical geography of your institution? Will it be possible for them to easily reach Code Blues called in different areas of the hospital?
Once you’ve identified potential candidates, you’ll need to get buy-in from department heads, executive leadership, and of course the individual team members themselves that they are willing to carry code pagers and respond.
With current staff considered and all willing, qualified candidates on board, how many gaps still remain between your confirmed team members and your “need” and ”want” lists? It may be necessary to hire or otherwise adjust staffing to ensure consistent coverage and responsiveness, which again will require executive and department head approval.1
When at last all critical team roles are filled, it’s time to set your resuscitation responders up for success.
Empowering your resuscitation response team
Data shows standardized Code Blue responses have the best outcomes.2 That’s why it’s important to empower your resuscitation response team with unified activation processes and regular, high-quality team training.
UNIFIED RESPONSE ACTIVATION
Every institution needs an easy, consistent way to activate an emergency response at any time of day. This process varies between institutions, but might look something like the following:
- All general staff learn how to place a Code Blue call to an emergency line. They relay the exact emergency, their own name, the location of the emergency, and a callback number. After getting an estimated response time, they return to the emergency to perform or assist with BLS while awaiting the code team.
- Emergency line operators collect this basic information from potentially very stressed staff members. They repeat the information back for confirmation and provide an estimate of when the code team will arrive. Finally, they page designated members of the resuscitation response team with all the pertinent info.
- Resuscitation response team members actively acknowledge the page and respond as quickly as possible to the location provided.
Furthermore, Code Blue responders should also work together to identify and address any barriers hindering team members from responding in a timely manner:
- Are there pager dead zones anywhere in the hospital, such as in Radiology? Perhaps a different code pager frequency or PA system could be used to alert staff in that department.
- What if a code team doctor is in a procedure and cannot run immediately to the emergency? Or a code team nurse is with a patient for a CT scan? Could a backup doctor or nurse carry the pager in these scenarios?
- Do staff have access to all areas of the hospital — including locked units?
These barriers need to be thought through, workarounds tested, and procedures put in place to ensure that responders can get where they need to go and work as a team consistently.
REGULAR TEAM TRAINING
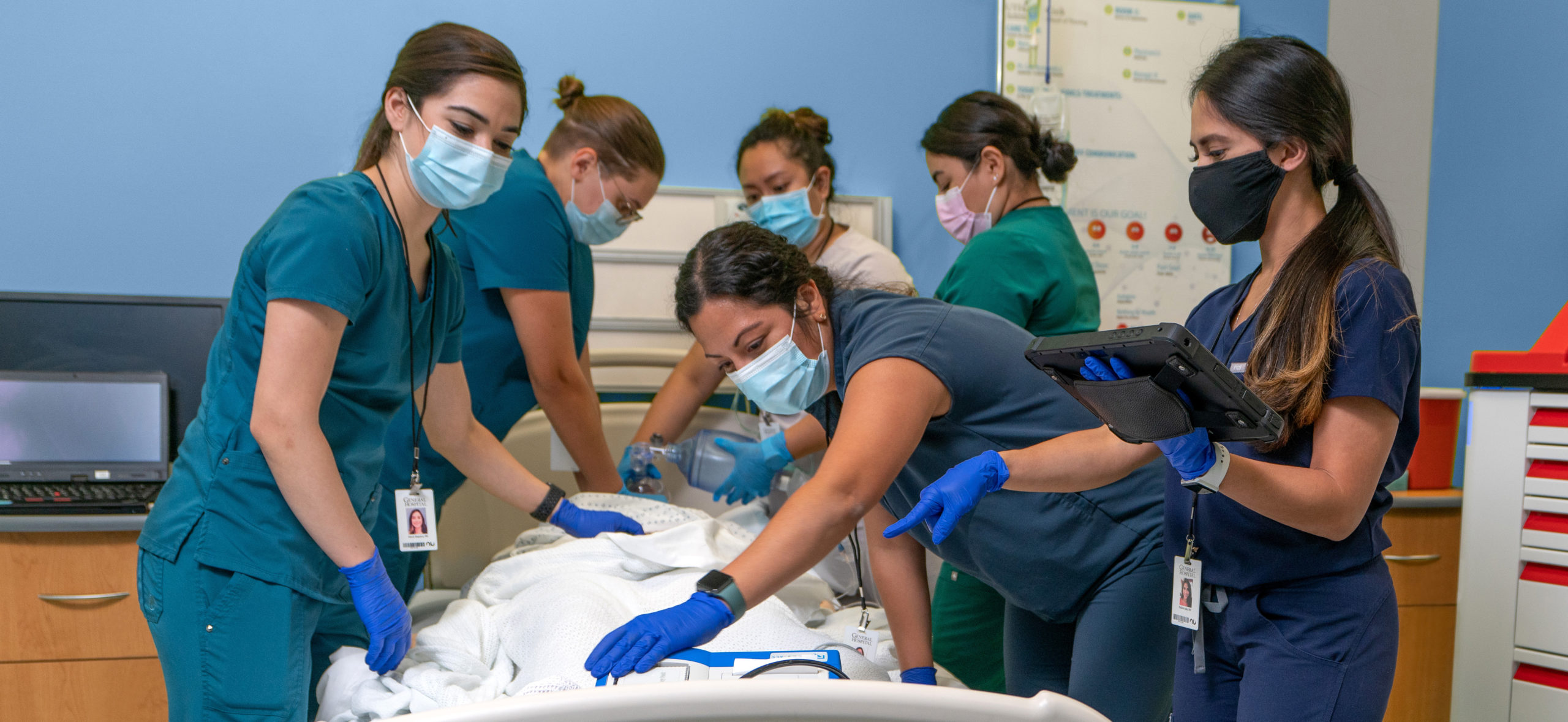
Simply having certified resuscitation response team members armed with pagers and ready for activation doesn’t mean they know how to work together as a team. One of the most effective ways to nurture collaboration and cement best practices is to hold in-situ mock codes.3
These training exercises simulate emergency situations and scenarios that every team member will need to be able to respond to with reflexive speed and practiced skill. Mock codes take place in the actual environment where responders work and involve all the same medications, supplies, equipment, protocols, and role expectations that will be in place during live Code Blue events.
By reinforcing skills, highlighting positives, and supporting opportunities for improvement, regular in-situ mock codes can help responders work together, learn from one another, and gel as a real, cohesive team.
Mock Codes Can Also Help You Comply with The Joint Commission’s Revised Resuscitation Standards
As of January 2022, The Joint Commission will require hospitals and critical care facilities to provide regular training and education to keep selected staff up to date on topics such as resuscitation procedures, protocols, techniques, and equipment.4
We’re Here to Help
With a consistent Code Blue response team supported by consistent activation and training, your hospital’s emergency response will be stronger — and your patient outcomes likely better. CoDirector® Software from Nuvara® can help by empowering responders to:
- Digitally document training events and results
- Train with real-time, data-driven mock code insights
- Compare mock code performance data against real events

RELATED ARTICLES
See for Yourself
CoDirector Software can help your hospital improve emergency response processes and comply with new resuscitation standards from The Joint Commission.
References
-
Prince, C. R., Hines, E. J., Chyou, P., & Heegeman, D. J. (2014). Finding the key to a better code: Code team restructure to improve performance and outcomes. Clinical Medicine & Research, 12(1-2), 47–57. https://doi.org/10.3121/cmr.2014.1201
-
Qureshi, S. A., Ahern, T., O’Shea, R., Hatch, L., & Henderson, S. O. (2012). A standardized code blue team eliminates variable survival from in-hospital cardiac arrest. The Journal of Emergency Medicine, 42(1), 74–78. https://doi.org/10.1016/j.jemermed.2010.10.023
-
Yager, P., Collins, C., Blais, C., O’Connor, K., Donovan, P., Martinez, M., Cummings, B., Hartnick, C., & Noviski, N. (2016). Quality improvement utilizing in-situ simulation for a dual-hospital pediatric code response team. International Journal of Pediatric Otorhinolaryngology, 88, 42–46. https://doi.org/10.1016/j.ijporl.2016.06.026
-
The Joint Commission. (2021, June 18). R3-report_resuscitation [PDF]. https://www.jointcommission.org/. Retrieved July 30, 2021, from https://www.jointcommission.org/-/media/tjc/documents/standards/r3-reports/r3-report_resuscitation_hap_final_.pdf