Per The Joint Commission’s latest resuscitation requirements, effective January 2022, hospitals must provide regular education and training to staff who are involved in the provision of resuscitative services (PC.02.01.11 EP4).
Each hospital must determine which staff complete this education and training based upon their job responsibilities and hospital policies and procedures. It’s also up to hospitals to decide when training and education should be provided, such as at orientation and/or during role changes and other applicable events.1 But in terms of how, we can turn to the American Heart Association (AHA) for resuscitation training best practices.
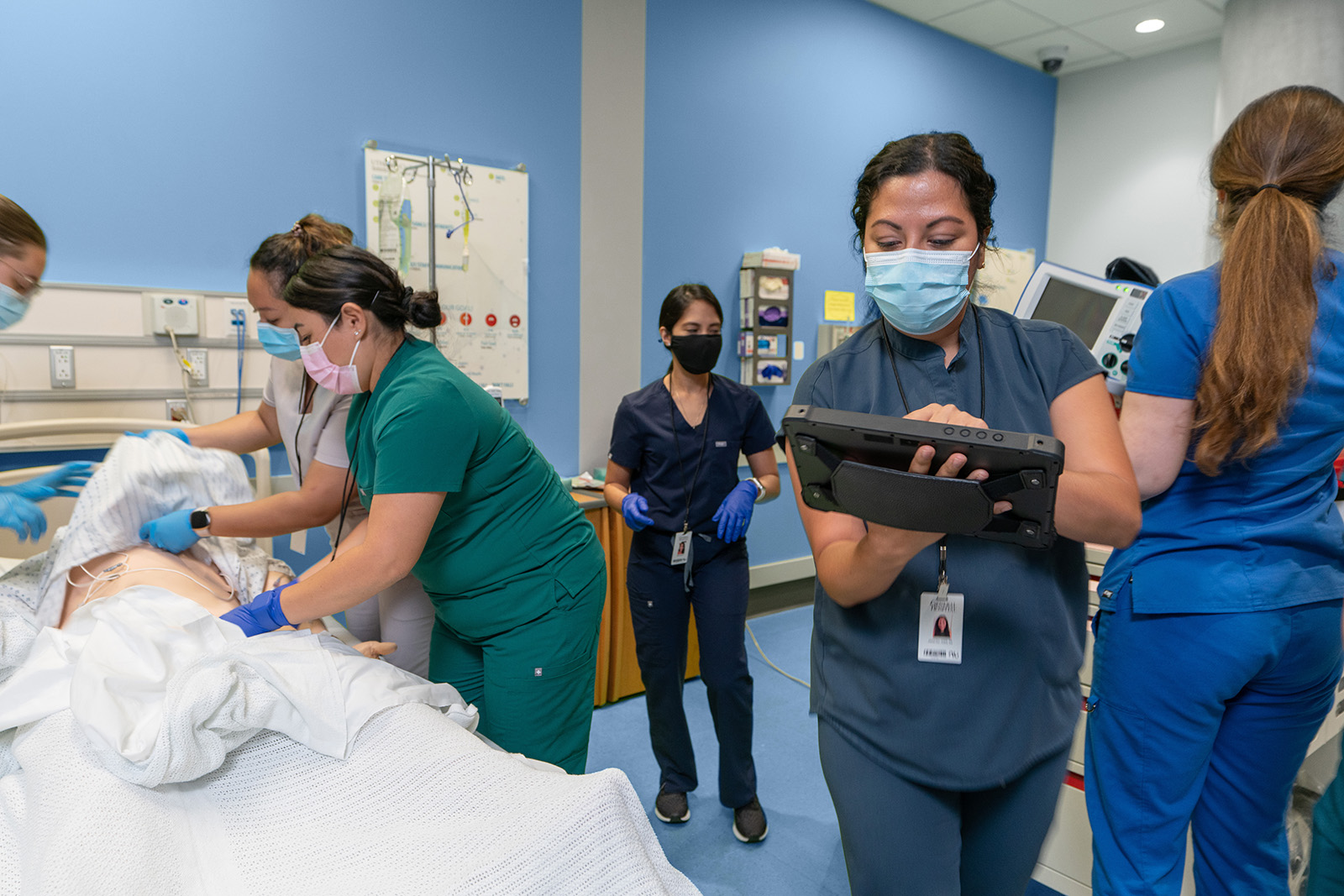
According to the AHA, simulating resuscitation events is one of the best ways to teach and reinforce these life-saving procedures. From learning about roles and responsibilities and how to work as a team to training on specific resuscitation techniques, these simulations allow responders to put critical skills into practice. They create a sense of reality without any risk to actual patients.
There are two main types of resuscitation simulations: high-fidelity (hi-fi) and low-fidelity (low-fi). Both types help Code Blue responders acquire, sharpen, and reinforce resuscitation skills and both require planning and coordination. But they are very different in terms of requirements, benefits, and drawbacks.2 Keep reading to learn more about the differences between hi-fi and low-fi Code Blue simulations — and which might be best for your hospital and clinical teams.
High-Fidelity Code Blue Simulations
Hi-fi resuscitation simulation is now recommended as baseline training for all nurses and doctors in school. These high-end training events have been shown to support realistic patient interactions while decreasing participant stress levels.3
They can help responders hone specific skills and tighten adherence to resuscitation response expectations, such as the AHA guidelines, based upon realistic physiological findings.
Requirements:
- Dedicated training space
- Highly realistic simulated patient
- Extensive variety of resuscitation training medications, supplies, and equipment
Benefits:
- Realism — Extremely realistic simulation patient can talk or even cry, and will typically have vital signs, invasive waveforms, and a pulse.
- Effectiveness — Extremely realistic environment can help clinicians practice required skills and roles during resuscitation events.
- Broader skill sets — Clinicians can practice intubation, placing chest tubes, administering medications, and defibrillation — and see immediate and realistic physiological responses.
Drawbacks:
- High cost — A single high-fidelity resuscitation simulation room can cost nearly $1 million.
- Inconvenience— Events typically take place in a simulation center set apart from actual clinical settings.
Low-Fidelity Code Blue Simulations
Low-fi resuscitation simulations, on the other hand, are typically extremely basic setups that can be conducted nearly anywhere on very short notice. They’re easily transported and offer clinical teams many of the same benefits of more expensive hi-fi simulations.
In fact, staff often prefer low-fi simulations conducted in the same facilities and with the same clinical teams they will actually encounter during Code Blue events, even if the simulated patient is not as realistic. This in-situ environment helps to build muscle memory of skills and roles for resuscitation events.4 Studies have even found that low-fidelity resuscitation simulation sessions can create better muscle memory and reinforce skills more effectively than hi-fi simulations.2
Requirements:
- Any training area
- Basic mannequin
- Training defibrillator
- Essential training meds
Benefits:
- Low cost — $1,000 would cover an extremely robust low-fi set up.
- Flexible location — Events can take place essentially anywhere, including in-situ within the actual hospital and department where staff will be responding to real Code Blue events.
- Highly effective — Build better muscle memory compared to hi-fi simulations.
Drawbacks:
- Less feedback — Trainees must rely on feedback from instructors (and/or each other) rather than getting physiological responses from a more realistic simulated patient.
What does this mean for your hospital?
Offering regular Code Blue simulations as part of a resuscitation training and education program can help your hospital align with The Joint Commission’s 2022 requirements. If you’re considering such a program, you essentially have three options.
- Hi-fi only: Off-site, high-fidelity resuscitation simulations can provide invaluable physiological feedback to help clinicians immediately understand the results of their actions and interventions. These sessions would likely be less frequent, as they are typically very expensive and harder to schedule.
- Low-fi only: Basic in-situ simulations might be a better option for your hospital if you have less budget to work with and/or if you have trouble wrangling schedules around off-site training events. These can be just as effective, and in some ways even more effective than hi-fi simulations.
- A mix of high- and low-fidelity: It may be preferable to schedule a hi-fi resuscitation simulation once per year with the opportunity for staff involved in resuscitation services to attend more frequent low-fi simulation events. This way, you could get the best of both worlds — frequent in-situ sessions to build team dynamics and skills related to your institution’s specific techniques, technologies, and equipment; plus occasional high-fidelity events to ensure clinicians get feedback from a hyper realistic simulated patient.
Regardless of your hospital’s training and education budget and schedules, there are simulation options available that will provide excellent initial training as well as reinforcement of skills, roles, responsibilities, and expectations.5
RELATED ARTICLES
See How Nuvara® Can Help
Our CoDirector® Software can help your hospital improve emergency response training and comply with new resuscitation standards.
References
-
Clark. (2021). R3-report_resuscitation_hap_final_ [PDF]. The Joint Commission. Retrieved September 1, 2021, from https://www.jointcommission.org/-/media/tjc/documents/standards/r3-reports/r3-report_resuscitation_hap_final_.pdf
-
Massoth, C., Röder, H., Ohlenburg, H., Hessler, M., Zarbock, A., Pöpping, D. M., & Wenk, M. (2019). High-fidelity is not superior to low-fidelity simulation but leads to overconfidence in medical students. BMC Medical Education, 19(1). https://doi.org/10.1186/s12909-019-1464-7
-
Labrague, L. J., McEnroe-Petitte, D. M., Bowling, A. M., Nwafor, C. E., & Tsaras, K. (2019). High-fidelity simulation and nursing students’ anxiety and self-confidence: A systematic review. Nursing Forum, 54(3), 358–368. https://doi.org/10.1111/nuf.12337
-
Brauneis, L., Badowski, D., Maturin, L., & Simonovich, S. D. (2021). Impact of low-fidelity simulation-based experiences in a pharmacology classroom setting in prelicensure graduate nursing education. Clinical Simulation in Nursing, 50, 43–47. https://doi.org/10.1016/j.ecns.2020.10.002
-
Halm, M., & Crespo, C. (2018). Acquisition and retention of resuscitation knowledge and skills: What’s practice have to do with it? American Journal of Critical Care, 27(6), 513–517. https://doi.org/10.4037/ajcc2018259