key takeaways
- Mechanical CPR offers benefits like high-quality compressions and reduced stress for responders, but comes with risk as well.
- A thoughtful, strategic rollout of mechanical CPR can help mitigate risk at your hospital.
- Top strategies include assigning a point person to place the device, practicing device application often, having safeguards in place during initial rollout, and analyzing data to improve.
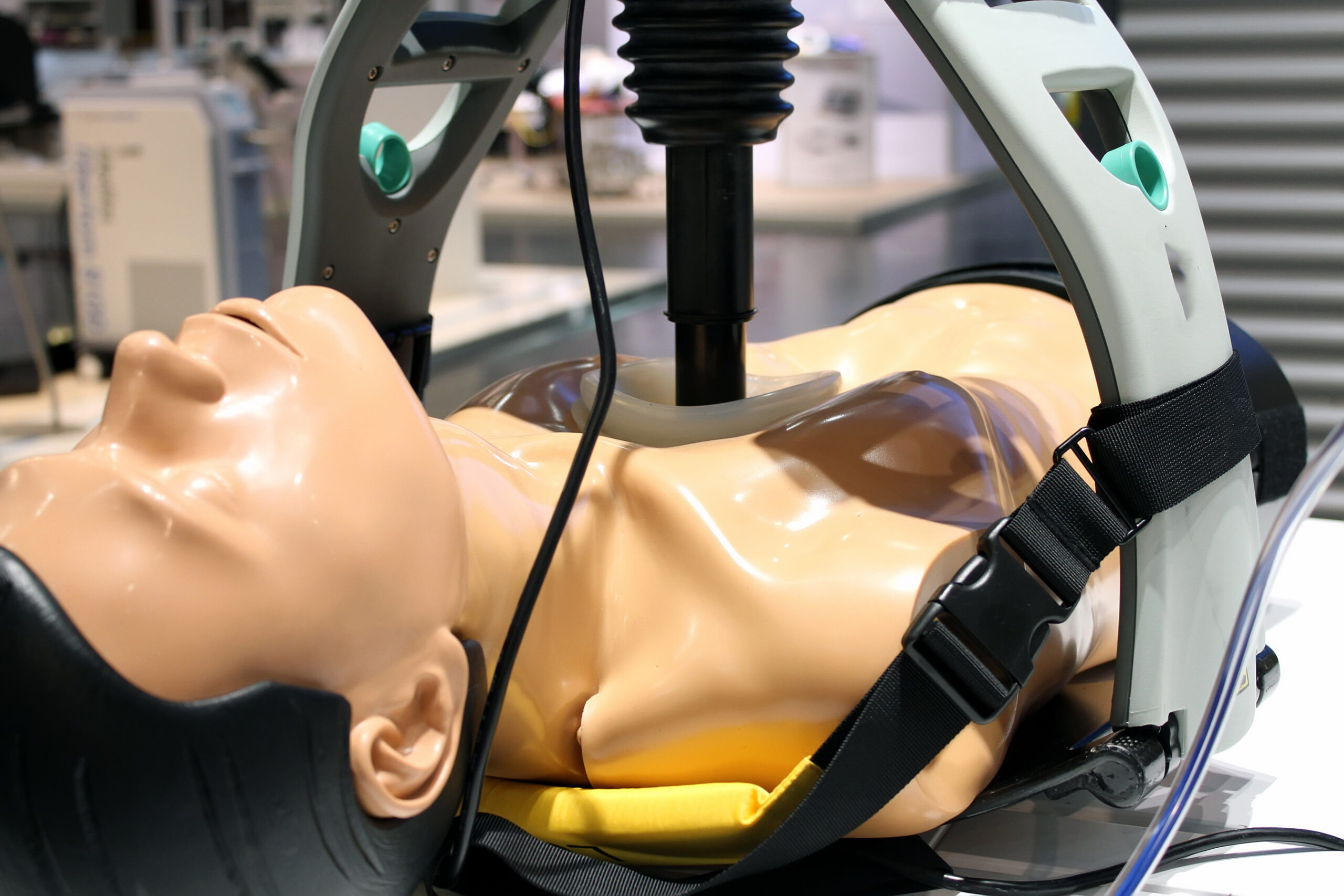
During the COVID-19 pandemic, use of mechanical cardiopulmonary resuscitation (mCPR) increased for in-hospital cardiac arrest (IHCA) as a way to deliver high-quality compressions while reducing the number of people in the room.1
Since that time, clinicians who use it have come to appreciate mCPR for other reasons as well: namely, for its role in providing a calmer, more controlled resuscitation experience all around.
Despite these benefits, mCPR is not without risk. Perhaps the most important risk for hospitals to be aware of is the potential for delay in lifesaving care — like chest compressions and defibrillation — while responders place the device.1,2
Here’s the good news: A thoughtful, strategic rollout of an mCPR program at your hospital can help mitigate this risk while maximizing the benefits. But what does that look like? Keep reading as we cover top strategies for hospitals to implement before, during, and after the rollout.
Before: Train & prepare
Obtain buy-in from all levels of staff
This includes everyone from administrators to nurses and other staff who will use the device during codes. Making sure staff members are well-versed in the benefits of mCPR can help. Common benefits include1-3:
- High-quality compressions
- Reduced overcrowding in the room
- Fewer interruptions to CPR with the ability to shock through compressions
- Decreased stress and burnout for clinicians
Create a protocol
A common pitfall is not assigning someone to place the device. Make sure your protocol includes how the device gets to the event and who is responsible for placing it.
Practice often
We recommend that your hospital begin training 3 months out. The goal is to allow plenty of time for staff members to learn and then fine-tune their process before going live. To avoid CPR delays, it’s especially important to have a well-rehearsed process for device application. Repetition is your friend: Have staff practice the steps for device placement until it becomes automatic: turning the device on, positioning the backplate, placing the device, etc.
During: Execute & mitigate risk
Determine fit
For greater accuracy, attempt to place the device instead of “eyeballing it” to determine if the patient will fit.
Reduce risk
During the initial rollout, allow patients to be shocked (as appropriate) before placing the device. Having safeguards like this in place can help prevent delays in care during growing pains with the new program.
Evaluate chest compression quality
Use a reliable, objective measure like end-tidal carbon dioxide (ETCO2) readings to evaluate compression quality. ETCO2 readings are helpful for post-code analysis (more on that in the next section), but they can also alert clinicians when something is off during the code. For example: Notable dip in ETCO2 readings during resuscitation? Have the team check to make sure the device is still positioned correctly.
After: Measure to improve
Analyze data
Use CPR data (depth, rate, chest recoil, hands-off time, etc.) to compare manual versus mCPR at your hospital. Doing so will likely highlight the benefits of mCPR and demonstrate concrete results to staff and administrators. Equally important, the data may also highlight any areas where additional training is needed.
Send a survey to staff after implementation
No rollout is perfect, and feedback will help your hospital determine in what areas staff need more support. Case in point: Although Beth Israel Deaconess Medical Center in Massachusetts managed to introduce mCPR rapidly during the COVID-19 pandemic with overall success, survey results still helped pinpoint specific areas where more training was needed.4 In their case, that included more experience using mCPR on different body types.4
RELATED ARTICLES
Keep reading
In case you missed it, check out our previous article on the history of mCPR and the pros and cons of its use for IHCA.
References
-
Mitchell OJL, Shi X, Abella B, et al. (2023). Mechanical cardiopulmonary resuscitation during in-hospital cardiac arrest. J Am Heart Assoc. https://doi.org/10.1161/JAHA.122.027726
-
Poole K, Couper K, Smyth MA, et al. (2018). Mechanical CPR: Who? When? How? Critical Care, 22:140, 1-9. https://doi.org/10.1186/s13054-018-2059-0
-
Morley P. (2018). Mechanical cpr in a new light: A new approach to the analyses of resuscitation studies. Resuscitation, 130, A1–A2.https://doi.org/10.1016/j.resuscitation.2018.06.016
-
Bhatnagar A, Khraishah H, Lee J, et al. (2020). Rapid implementation of a mechanical chest compression device for in-hospital cardiac arrest during the COVID-19 pandemic. Resuscitation, 156, 4–5. https://doi.org/10.1016/j.resuscitation.2020.08.122